Abstract
Pediatric transfusions account for 5-10% of all blood transfusions administered across the country and 4.8% of hospitalized children required blood transfusions in a multicenter study across pediatric academic centers. However, studies using validated assessment tools have shown low levels of knowledge and comfort about transfusion medicine (TM) practices among residents in training across different medical specialties, including pediatrics. Most residency programs do not offer a TM curriculum, and there is paucity of data on the impact of such a curriculum in pediatrics. The primary objective of our study was to assess the impact of a structured TM curriculum on the knowledge of pediatric residents regarding TM.
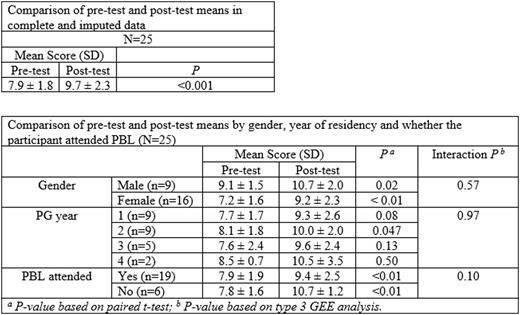
A curriculum was developed collaboratively by blood bank specialists and pediatric hematologists at our institution, covering essential topics previously validated by Haspel et al (Transfusion 2014) for assessment of physician TM knowledge. Problem-based learning (PBL) is known to improve the utilization of skills in clinical practice and hence, the curriculum was delivered as an interactive 40-minute lecture followed by an 80-minute PBL session, the latter utilizing case vignettes. All the pediatric residents who consented to the study underwent BEST-TEST3, a 21-question exam validated for assessment of TM knowledge among pediatric residents by Wheeler et al (Transfusion 2021). The test scores were assessed before and after the delivery of the curriculum (pre-test and post-test respectively). Paired sample t-test was used for univariable comparison of pre- and post-test scores, and the generalized estimating equations (GEE) models that account for within subject correlations were used to explore the modifying effect of covariates.
Out of 58 residents who attended the curriculum, 25 pediatric residents consented for the study and gave both the pre-test and post-test. Two residents were unable to attend the lecture but were provided access to the slides, and 6 residents did not attend the PBL session but were provided sheets with related information later. The mean score (standard deviation) improved significantly from 7.9 (1.8) before to 9.7 (2.3) after the the curriculum was completed(P <0.001). The improvement in test scores did not depend on gender, the year of residency, and the attendance of the PBL session (all interaction P > 0.10).
The mean pre-test score of 7.9 in our study, which is equivalent to 37.6%, is similar to the results of the international study by Wheeler et al that assessed pediatric resident knowledge using the same test (37.1%). A previous study showed an improvement in the test score by 2.7 points after 5 half-day sessions of lectures and team-based learning, compared to an increase of 1.8 points in our study. Given the limitations of time and subject experts to dedicate to resident teaching at most academic institutions, the format of TM educational material used in our study may be considered at other centers for effective as well as practically feasible delivery of TM related knowledge to pediatric residents.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.